Meso is an open source technology platform for health coverage administration.
Countries around the world have committed to digitizing their health systems in pursuit of universal health coverage (UHC). Meso was built to help make this possible.
How it works
Meso’s suite of mobile and web applications support each of the essential steps for administering a health financing system.
Enrollment
Easily enroll members, collect personal information and biometrics, and issue membership cards.

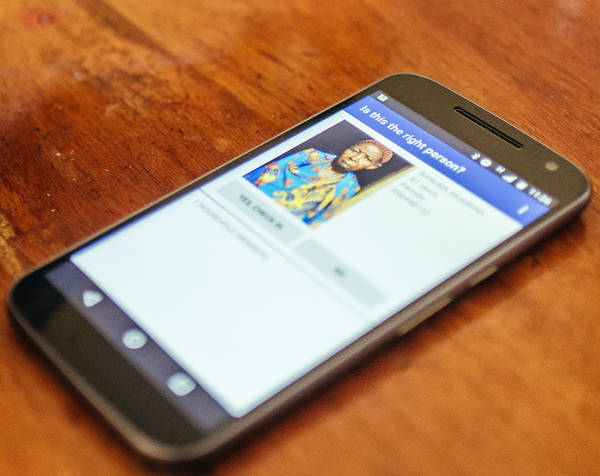
Identification
Accurately identify members, edit their personal information, and confirm their eligibility for services.

Claims submission
Efficiently collect claims and any corroborating documents from clinics, pharmacies, and hospitals.
Claims processing
Thoroughly review and adjudicate claims, and manage the provider reimbursement process.

Reporting
Intelligently analyze data across the entire system and make any necessary changes.


Benefits
Meso harnesses the power of data to reduce costs, streamline administration, and improve the quality of care.
Reduce cost
Identify fraud and surface data to reduce financial and operational waste.
Streamline administration
Increase efficiency and remove manual paperwork to ensure the consistent, timely delivery of both care and funds.
Improve quality
Leverage analytics to improve purchasing, policy, and experience for patients, providers, and staff.
Features
Meso is built to meet the complex needs of universal health coverage.
Scalable
Leverages proven technical infrastructure to scale quickly without compromising performance.
Secure
Adheres to current international best practices with regard to data privacy and security.
Flexible
Modular and easily adapts to meet the needs of different health insurance systems.
Intuitive
Built alongside payers, providers, and patients, to improve ease of use and reduce the need for training.
Interoperable
Architected to integrate with different systems and third-party clients such as EMR’s, HMIS’s, and mobile payments.
Robust
Developed for use in any setting, even if there’s limited internet connectivity or intermittent power.


